Midline, Loss of Resistance to Saline (LORS) Technique
Position the patient carefully
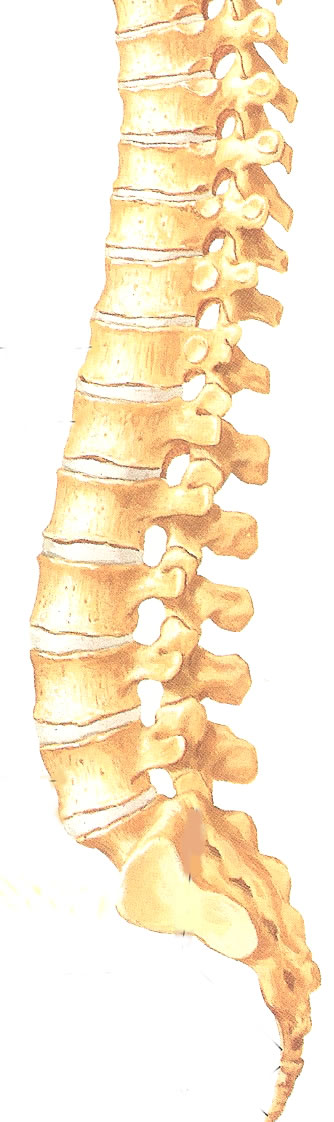
Mark the desired level using the landmarks described in the anatomy section as a guide.
For labour, gynaecological surgery and lower limb surgery select a lumbar level.
For abdominal and thoracic surgery select a thoracic level. As a guide, the level should correspond to a dermatome near the middle of the incision.
Choose a space that is easy to feel.
Use full aseptic technique including gown, gloves and mask.
Prepare the patient's back with alcohol and chlorhexidine and allow it to dry.
Drape the back
Inject lignocaine using the 23G needle into skin. In obese patients you can use the needle to help you find the space. Wait for the local anaesthetic to work. You can use the wait to draw up your saline into the loss of resistance syringe, draw up your local anaesthetic, flush your epidural catheter and filter.
Finally you get to pick up the Tuohy needle. Ask the patient to remain still. Insert the needle in the midline at 90 degrees for lumbar levels or aim slightly cephalad for thoracic levels. (INSERT PICTURE)
Compared to a spinal needle you may notice that the epidural needle requires more force to advance and gives more feed back about the structure you are in.
The first resistance you will feel after you are through the skin is the supraspinous ligament. Advance the needle further into the interspinous ligament. Classically, you should continue to advance the needle until you feel the "gritty" ligamentum flavum and an increase in resistance before attaching your LOR syringe. In reality, the ligamentum flavum isn't always easily recognized and the LORS technique works just as well if you start in the interspinous ligament.
At this point remove the plastic stylet in the needle and attach you saline filled LOR syringe. You should use you non-dominant hand to grip the needle. Brace the dorsum of your hand against the patient's back so that if the patient moves the needle does not advance. With your dominant hand compress the syringe and slowly advance the needle. You will feel a sudden loss or resistance and your syringe will empty a little. Stop advancing, you are in the epidural space. Make a note of the depth.
It is normal for a few drops of saline to drip out the needle. Wait for this to stop to ensure it isn't CSF. Next thread the catheter to about 15cm so that you don't pull it out when you withdraw the needle. NEVER pull the catheter back through the needle. The needle may shave the catheter tip off making it irretrievable. After withdrawing the needle, pull the catheter back so that only 3-5cm remains in the epidural space.
Attach the connector and filter to the end of the catheter. Aspirate gently for blood or CSF. If clear inject 5mls of 0.2% Ropivacaine and 100mcg Fentanyl.
Attach a water proof dressing of your choice and tape everything securely.
In labour ward you will want to establish a block immediately. 5mls of 0.2% ropivacaine intrathecally will usually cause a dense block so if the patient has no block inject another 5-10mls. You usually need about 15mls of 0.2% ropivacaine.